Leading Productive Meetings: A Pathway to Influence for Women in Healthcare
Meetings are more than just obligations that fill our calendars. They are opportunities to demonstrate leadership abilities and drive meaningful progress. For women in healthcare, in particular, maximizing this opportunity gives you a chance to demonstrate effective...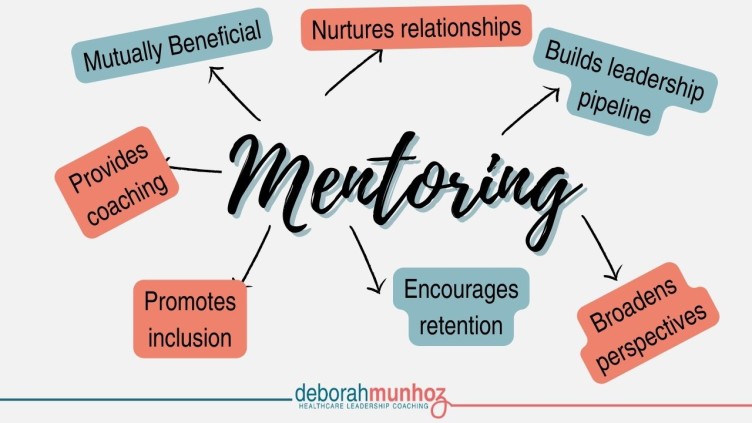
Women: Take Mentorship Into Your Own Hands
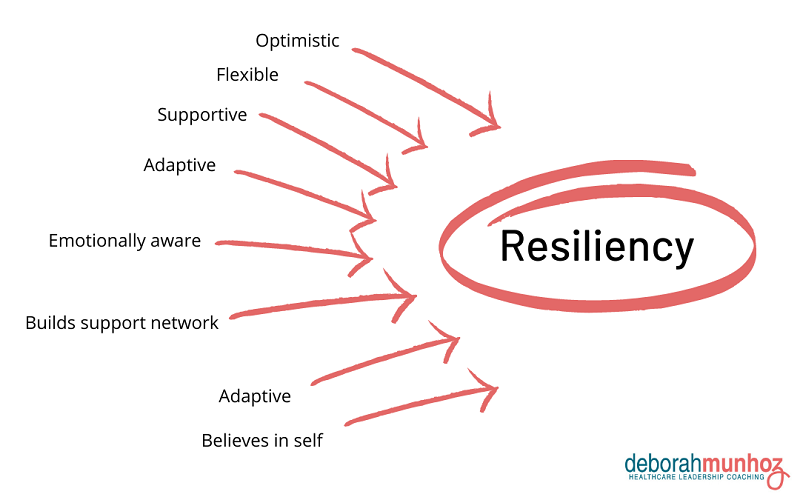
For the past year, to enhance my coaching practice, I have been conducting research about what barriers women physicians face. The data reflects four main areas that were the most common themes for women leaders in the healthcare industry: Mindset – This barrier shows...
Fix imposter syndrome in your workplace by shifting the conversation to “why does my employee feel this way?”
Baby Boomer women began entering the workforce in droves starting in the early 1960s. A few years later in 1978, psychologists Pauline Rose Clance and Suzanne Imes coined the phrase Imposter Syndrome to describe feelings of self-doubt many leaders experience,...
Curious Physician Leaders Find Creative Solutions to Healthcare Challenges
As you review your strengths as a leader in the healthcare arena, where does curiosity fall on your list? That’s right, curiosity. A recent Forbes article talks about how companies are actively seeking ways to recruit leaders who “explore new experiences and discover novel possibilities.”